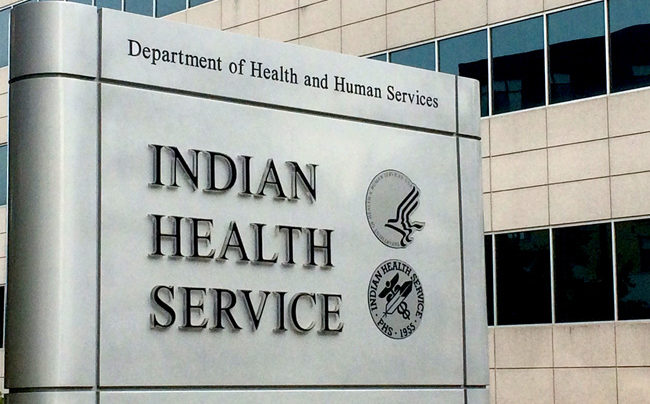
WASHINGTON, D.C. – During the recent World Alzheimer’s Day on September 21, the Indian Health Service (IHS) reaffirmed its commitment to building tribal and urban Indian health system capacity to address Alzheimer’s disease and related dementias by announcing $1.5 million in new cooperative agreements.
The IHS Alzheimer’s Grant Program 2023 awards represent a continued investment in locally developed models that incorporate comprehensive approaches to care and service for American Indian and Alaska Native people living with dementia, and for their caregivers.
“Almost everyone knows someone with Alzheimer’s disease or dementia. Unfortunately, many American Indian and Alaska Native people, their caregivers, and their families suffer in silence as the disease takes a devastating toll,” said IHS Director Roselyn Tso. “With this additional funding, we bring resources to eight new communities to begin to increase awareness and recognition of the disease and improve the systems of care and services.”
After its pioneering allocation of funds last year, the IHS remains steadfast in its mission to support those facing dementia challenges in tribal communities, including both undiagnosed and diagnosed patients and their caregivers. These new awardees join current 2022 recipient’s efforts to continue designing and executing locally developed, innovative models that prioritize culturally competent screening, diagnosis, and management of persons living with dementia and their caregivers.
The 2023 cooperative agreement awardees include:
- Absentee Shawnee Tribal Health System (Oklahoma) – $199,928 – aims to refine its patient-focused dementia care system for the rural, non-reservation, American Indian community, establishing a foundation for a culturally tailored treatment and broadening dementia care services, mitigating symptom effects on tribal elders, enhancing caregiver well-being, and decreasing health care expenses.
- Cherokee Nation Health Services (Oklahoma) – $198,250 – will use grant funds to hire a patient services advocate, enhancing comprehensive dementia care by offering dedicated support to patients and caregivers, coordinating outreach, increasing awareness and early diagnosis, facilitating educational resources, and fostering community partnerships to benefit those affected by dementia.
- The Cheyenne and Arapaho Tribes (Oklahoma) – $200,000 – will implement a new program to improve dementia support for Cheyenne and Arapaho tribal members. It will provide assessments, caregiver assistance, training for the Healthy Aging Team, and collect data on cognitive impairment prevalence.
- The Confederated Tribes of Grand Ronde Community of Oregon (Oregon) – $198,603 – are unveiling a comprehensive, culturally tailored dementia program to address the growing needs of their community, focusing on early detection, caregiver support, and holistic wellness.
- The Fallon Paiute-Shoshone Tribe (Nevada) – $146,422 – will hire a dementia care specialist, assess dementia prevalence in the Fallon Paiute-Shoshone service area, identify care gaps, and introduce a culturally relevant, community-based care model guided by a Dementia Care Steering Committee from various tribal health organizations, while also promoting public education and establishing caregiver support groups.
- The Kenaitze Indian Tribe (Alaska) – $164,179 – introduces a comprehensive dementia care program for tribal elders, combining interdisciplinary care, thorough oversight, and commitment to sharing insights.
- The Norton Sound Health Center (Alaska) – $200,000 – will utilize the grant to hire staff for coordinating patient assessments, referrals, and multidisciplinary team efforts, collaborating with regional tribal and community services, sharing best practices with IHS programs via the Alaska Native Tribal Health Consortium, and exploring funding options including a pilot program for respite care.
- The Seattle Indian Health Board (Washington) – $199,881 – aims to amplify culturally resonant, holistic dementia care for American Indian and Alaska Native individuals in Seattle/King County, integrating traditional Indian medicine, and will share insights with urban Indian organizations to address the unique needs of urban Native elders, caregivers, and health care providers.
As many as one in three American Indian and Alaska Native people ages 65 and older are at risk of developing dementia. Today, one of every six American Indian and Alaska Native adults ages 45 and older reports experiencing subjective cognitive decline, which can be an early sign of progressive memory loss. At the same time, younger Native people experiencing early symptoms of memory loss are disproportionally affected by high rates of co-occurring chronic diseases like heart disease, diabetes, and kidney disease.
As many as six in 10 older American Indian, Alaska Native, Hispanic, and other historically underserved groups with probable dementia have either not been diagnosed or remain unaware of their condition. The IHS is steadfast in its dedication to collaborating with various federal agencies and non-governmental organizations. This collaboration aims to enhance initiatives related to Alzheimer’s disease and associated dementias, with a particular focus on workforce training and community outreach.
In addition to this award announcement, the IHS Alzheimer’s Grant Program highlights the remarkable accomplishments of the fiscal year 2022 Indian Health Geriatric Scholars’ debut cohort. Fifteen physicians, nurse practitioners, physician assistants, and pharmacists recently concluded first-year GeriScholar activities, culminating in presentations detailing their efforts to improve the care of the older adults they serve. Furthering their commitment to excellence in geriatric care, IHS is unveiling the induction of 16 new participants into the Indian Health GeriScholars pilot for FY 2023. Inspired by the highly regarded VA Geriatric Scholars Program, this initiative commits to enhancing the expertise of IHS, tribal, and urban Indian health professionals. Representing seven IHS regions, these scholars will benefit from immersive training and specialized clinical practicums in geriatrics and will spearhead quality enhancement endeavors in their respective facilities.